On August 14th, the New England Journal of Medicine published three studies looking into dietary sodium and the implications this has on blood pressure, cardiovascular disease and premature mortality. On Tuesday, September 9th, NephJC discussed these studies.
The full transcript and analytics are available here:
Study #1 (Pubmed link) and Study #2 (Pubmed link) are from the PURE study group, based at McMaster in Hamilton, which has as its aim the study of societal influences on non-communicable diseases. Study #3 (Pubmed link) is somewhat different, from Mozafarrian and colleagues from the NUTRICODE study group, and using complex modelling techniques, it tries to estimate the global impact of high sodium intake.
NephJC co-founder, Joel Topf, has summarized the three studies on his blog PBFluids.com in his signature style, and his posts are reproduced below.
Association of Urinary Sodium and Potassium Excretion with Blood Pressure
The first article is the Association of Urinary Sodium and Potassium Excretion with Blood Pressure. This question used the large epidemiologic study, Prospective Urban Rural Epidemiology (PURE) to answer the question.
PURE enrolled 157,543 adults age 35 to 70 from 18 low-, middle-, and high-income countries on 5 continents.
The study collected 102,216 fasting first morning urines. The authors used the Kawasaki formula to extrapolate 24 hour urine sodium and potassium from the samples. They collected 24-hour samples on 1,000 patients and found that they over estimated sodium intake by about 7%:
The mean sodium excretion was 4.9g and the mean potassium excretion was 2.1 grams.
It was difficult for me to understand the difference between the Observed excretion and Usual excretion but the authors seemed to reference the Usual excretion as the definitive curve.
Sodium excretion was higher in rural areas and in lower income countries. The reverse was true for potassium, higher in cities and higher in higher income countries.
The meat of the paper was the positive association between sodium intake and blood pressure. For every additional gram of sodium excretion the systolic blood pressure went up 1.46 mm Hg and the diastolic rose 0.54 mm Hg (P less than 0.001). Statistical mumbo jumbo increased those numbers to 2.11 systolic and 0.78 mm Hg diastolic. This relationship was non-linear with increased blood pressure effect as the sodium excretion rose over 5 grams.
Potassium had the opposite effect with systolic blood pressure falling 0.75 systolic (1.08 after statistical adjustment) and diastolic dropping 0.06 (0.09 adjusted) mm Hg for every gram increase in potassium excretion.
Older people showed larger changes in blood pressure with increased sodium excretion.
The sodium effect on blood pressure was a lot larger that the 0.94 mmHg systolic and 0.03 mmHg diastolic found in the landmark INTERSALT study but still seems like a pretty small effect given the difficulty in getting to a low a salt diet. Look at the bell curve showing only 0.2% of samples hitting the WHO goal of less than 2.3 g a day.
Urinary Sodium and Potassium Excretion, Mortality, and Cardiovascular Events.
The second article in the NEJM package was Urinary Sodium and Potassium Excretion, Mortality, and Cardiovascular Events.
This is an interesting study because so much of the arguments based on salt focus on the intermediate end-point of blood pressure, one can lose sight on the big daddy, total mortality. Previous studies have shown that low sodium diets have paradoxically been associated with higher rates of cardiovascular disease and death. These studies have often been dismissed by sodium puritans by pointing out that including patients with pre-existing cardiovascular disease will pollute the results because these, obviously, high risk patients are told to maintain a low sodium diet.
This study was performed using the same international cohort as the previous trial, The PURE study. This study enrolled 101,945 patients and analyzed early-morning fasting urine samples. They used the same Kawasaki formula that over estimated sodium excretion as in the other PURE study.
They used multiple models to analyze the data.
Patients with pre-existing cardiovascular disease, cancer or events in the first two years of follow-up were excluded from the analysis. They also did an additional analysis using propensity scoring to further reduce imbalanced confounders.
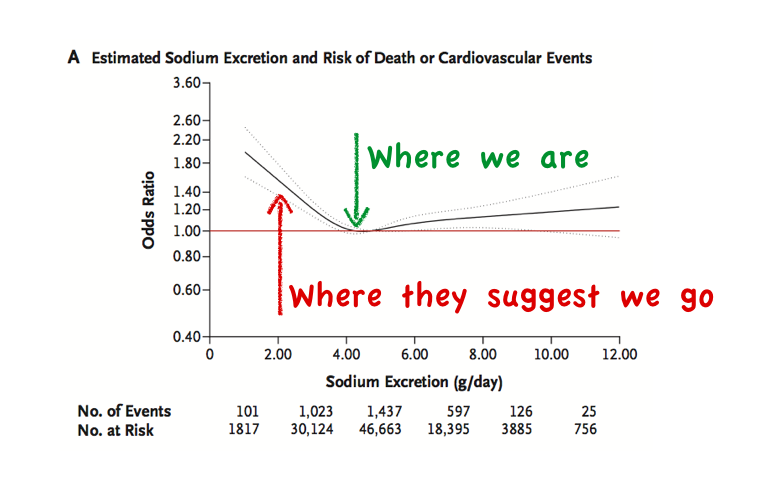
The most important letter in the PURE acronym is P for prospective. In this case it allowed them to match the cross sectional sodium excretion data with long-term follow data. Mean follow-up was 3.7 years. The primary outcome was death or a major cardiovascular event. Over the period covered by the study they recorded 3,317 outcomes. The risk from changes of sodium intake was seen at the edges of intake:
Increased mortality at sodium excretion over 7 grams and below 3 grams
Green indicates an association with sodium excretion. Red indicates no significant association.
The U-Shaped curve seen with sodium was not seen with potassium. The more potassium excretion the lower the risk of the primary outcome.
The results were essentially the same in the propensity-score-matched analysis.
I found this paragraph from the discussion to be particularly salient:
Current guidelines, which recommend a maximum sodium intake of 1.5 to 2.4 g per day, are based on evidence from largely short-term clinical trials showing that reducing sodium intake from a moderate to a low level results in modest reductions in blood pressure. The projected benefits of low sodium intake with respect to cardiovascular disease are derived from models of data from these blood-pressure trials that assume a linear relationship between sodium intake and blood pressure and between blood pressure and cardiovascular events. Implicit in these guidelines is the assumption that there is no unsafe lower limit of sodium intake. However, sodium is known to play a critical role in normal human physiology, and activation of the renin–angiotensin–aldosterone system occurs when sodium intake falls below approximately 3.0 g per day.
The authors make it clear that an epidemiologic association between mortality and sodium excretion is not the same as finding increased mortality or lack of benefit from patients lowering their sodium intake. Advice that the authors of the third study should have taken the time to internalize.
Finally, our study provides an epidemiologic comparison of groups that consume different levels of sodium, and it does not provide information on the effect on clinical outcomes of reducing sodium intake. Therefore, our findings should not be interpreted as evidence that the intentional reduction of sodium intake would alter the risk of death or cardiovascular disease.
Global Sodium Consumption and Death from Cardiovascular Causes
The last article in NEJM's remarkable sodium package is an extraordinary analysis attempting to estimate the number of deaths that can be attributed to excess sodium intake.
Global Sodium Consumption and Death from Cardiovascular Causes.
The authors reviewed 205 studies of dietary sodium consumption:
142 studies that used 24-hour urine collections
91 with estimates of dietary intake
28 with both methods
These studies came from 66 countries representing 74.1% of the adult population. It is appropriate to whistle and say wow, at this point.
In order to translate the sodium intake into mortality the authors first needed to estimate sodium's effect on blood pressure. They employed two Cochrane meta-analysis looking at the effect of reduced sodium intake on blood pressure (Meta 1, Meta 2). They used these meta-analysis to discover sources for there own meta-analysis. They needed age and gender specific effects of sodium on blood pressure which is why they needed to do their own analysis.
After estimating the effect of sodium on blood pressure, they then used the blood pressure data to estimate cardiovascular mortality based on the work done in two large studies (Study 1, Study 2).
Estimated global sodium intake was 3.95 g per day, quite a bit lower than the 4.4 grams measured in the PURE studies. They pointed out that 99.2% of the countries surveyed had mean sodium intakes higher than the WHO level of 2 grams a day. An astounding 88% of the world had sodium intake more than 50% over the WHO recommendation.
Their meta-analysis found that systolic blood pressure fell 3.8 mm Hg for every 2.3 grams sodium intake was reduced. This translates to a more interpretable 1.6 mm Hg for every gram reduction in sodium. This is quite close to the 1.5 mm Hg found in the PURE analysis. They used 2.3 grams because that is equal to 100 mmol of sodium, for people who like to speak like a chemist.
They then ran the blood pressure data into the mortality data from blood pressure and concluded that consuming more than 2 grams of sodium a day results in 1.65 million deaths from cardiovascular disease a year. This is 9.5% of all cardiovascular deaths in the world and nearly 20% of all premature deaths.
However, despite a very through analysis this is an exercise in somewhat meaningless statistical gymnastics. The authors fail to consider the possibility that lowering the blood pressure too far could have negative consequences, (Hello ACCORD Trial. Nice to meet you.) Or the possibility that low sodium diets could be harmful.
Note that, these figures come from a 2011 prospective trial published in a little known journal called JAMA. This signal that low sodium diets may not be beneficial is not new or unknown. It was picked up by the Institute of Medicine in their summary and recommendations to avoid very low sodium diets:
However, the evidence on health outcomes is not consistent with efforts that encourage lowering of dietary sodium in the general population to 1,500 mg/day. Further research may shed more light on the association between lower—1,500 to 2,300 mg—levels of sodium and health outcomes.
This becomes even more concerning when looked at through the lens of the PURE studies in the same issue of The Journal that show average sodium intake to be associated with the lowest mortality and danger rising on either side of the sodium consumption curve.
This is a study best taken with a grain of salt. Couldn't resist.
Feel free to get involved by joining the live Twitter chat on Tuesday 9th September at 9pm Eastern using #NephJC.