In the 1950s, there was a deluge of advertisements showing physicians being poster boys/ girls for cigarette smoking. I suppose, tobacco corporations figured that, if physicians, who were considered as noble, all-knowing and infallible, consumed tobacco, then the common man in the streets would follow suit. In some cultures, physicians had a god-like stature due to their dedication to the good of mankind and nothing else. There was a time when whatever physicians say or did, was regarded as gospel.
This is paternalism in medicine.
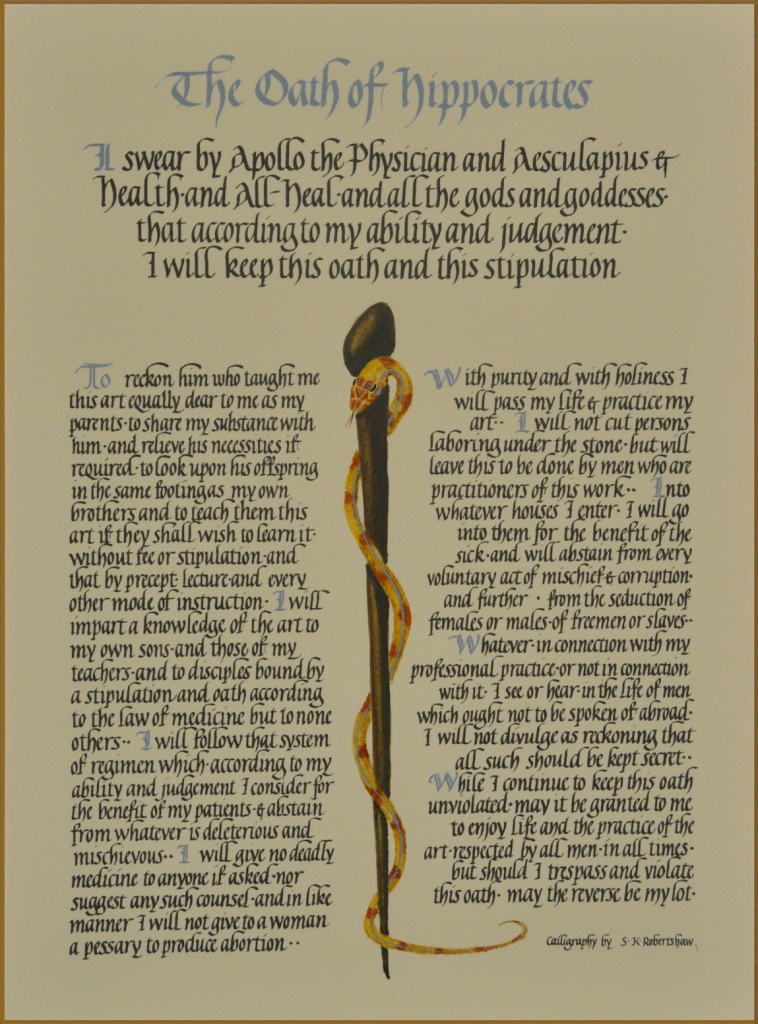
However, paternalism in medicine goes well beyond the 1950s. In fact, Hippocrates, the father of medicine, can also be considered, the “father of medical paternalism.” Proof lies in the ‘Hippocratic Oath,’ which is recited by medical students as they transition to full-fledged physicians.
When one truly understands the oath, the paternalism is quite noticeable by some uncanny omission of certain important ethical principles. In Dr. Robert Shmerling’s blog he alludes to the following ‘overt’ omissions:
- Honoring patients’ preferences
- Sharing medical information with patients
- Avoiding conflicts of interest, such as ordering profitable but unnecessary tests and treatments
- Protecting patients who enroll in research studies
- Treating all patients equally, regardless of ability to pay, social class, education, race, or suspicion of criminality
- Avoiding the practice of medicine while impaired (due to physical or psychological disease).
So, in this age of modernization and digital technology, is the Hippocratic Oath still valid in its entirety?
Despite the known pitfalls and negative implications of paternalism, this tradition continues to pervade medical practice in multiple ways:
INFORMATION ASYMMETRY refers to the while physicians have access to all the data, information and knowledge, patients are maintained as passive participants in the doctor-patient relationship. The author feels that the terms doctor’s orders and patient have negative connotations. The former implies having some sense of god-like authority and supremacy, while the latter refers to passivity. Think about it: as an adjective, patient is defined as able to accept or tolerate delays, problems or suffering without being annoyed or anxious.
INFORMED CONSENT. Topol describes informed consent as quasi- or pseudo-informed because, most individuals don’t actually read the whole document before signing it.
GUIDELINES. Professional organizations create guidelines which define the standard of care. Despite the provision that such guidelines are not intended to be dictatorial, and that individual patients merit consideration, there are some legal implications attached. Emily Oster points out that paradoxically, patients can face grave risks when doctors adhere to the guidelines.
In this chapter, Topol brings up the guidelines on statins issued in November 2013 by the AHA/ ACC as an example of the problem. I think the recent JNC VIII Hypertension Guidelines also fall under this conundrum.
The table below list several guidelines for routine testing or diagnosis that been questioned or overturned in the past several decades.
In this day and age of modernization and technology, we are also seeing the advent of the “individual, active patient.”
In this digital age, where everyone has a smartphone or a tablet, access to information is a given. However, paternalism will need to be eliminated for all patients to be able to have complete and uninterrupted access to such information. The end of paternalism simply means that patients are ‘actively’ involved in their medical care, from diagnosis to treatment; they are able to ask questions without fear of any repercussions; they are able to express their feelings openly, e.g., decline recommended treatments, seek second and third opinions about every aspect of medical care.
Nowadays, we don’t see advertisements with physicians being models for tobacco consumption. Instead, we see this. The Surgeon General’s Warning came as a collaborative effort of physicians as well as individual “active” patients who expressed their viewpoints based on what they’ve learned and understood.
Topol states that , “For this (end of paternalism) to occur, it will require not only a change in culture within the medical community, but also new technology to drive it from outside, like the printing press did several hundred years ago.”
That new technology is here…the culture change will need to gain momentum.
The time-honored doctor-patient relationship is not a one-way but a two-way street.