#NephJC chat
9 pm Eastern Tuesday August 23
8 pm BST 12 noon Pacific Wednesday Aug 24
2016 Jul 14. pii: ASN.2016030248. [Epub ahead of print]
Red Meat Intake and Risk of ESRD
Lew QJ, Jafar TH, Koh HW, Jin A, Chow KY, Yuan JM, Koh WP
PMID: 27416946 Get it for free here: courtesy JASN, till August 31st
UPDATE [Aug 22 2016]: JASN also has an editorial, out today from Drs Goraya and Wesson. Read it here: JASN Red Meat editorial (gated)
Introduction
If I had a Loonie/pound/dollar/euro for every time a patient in clinic had asked me, “Is it what I eat doctor?” when I had told them that their CKD had progressed, I would have at least enough Loonie/pounds/dollars/euros to treat myself and a few colleagues to dinner. The question I ask myself after reading this paper is: would I avoid the steak? Glib introductions aside, this is an important issue for nephrology for two reasons.
Firstly, attempts to unpick the relationship between dietary protein and CKD progression have a distinguished history. Like any topic with a prodigious literature, both sides of the argument are well represented and for many the failure of the MDRD study to demonstrate a benefit of protein restriction on CKD progression remains the key result. The current KDIGO CKD guidance is to lower protein intake to 0.8g/kg/day when GFR is less than 30ml/min (a good meal plan is here courtesy of one of UK’s leading renal dietitians: Jan Flint) and to avoid > 1.3g/kg/day in CKD “at risk of progression.”
Secondly, this genuinely is the question I am asked most frequently by patients about CKD. A casual google of “CKD” produces lots of conflicting advice on what to eat to preserve or even improve kidney function, so some knowledge in this area is key to practicing nephrology and empowering patients to look after their diet and their health.
The Study
This paper uses both the Singapore Chinese Health Study (SCHS), a prospectively collected population cohort of Chinese adults aged between 45 and 74, and the Singapore Renal Registry, to follow 60,198 individuals for a mean of 15.5yrs. The SCHS is a comprehensive record of health needs and includes a well-studied, quantitative, food-frequency questionnaire which allows accurate food intake estimates. However (somewhat surprisingly), no laboratory measures are included (not even creatinine or eGFR).
The group looked at total protein intake. They found an association between protein intake and incidence of ESRD (Table 2). However, the strength of the association varies depending on the covariates included in the model and is not significant when lifestyle and comorbidities are included.
Next, they shifted focus to different food sources of protein (Table 3) and found a dose dependent, positive association, of red meat intake and ESRD. This persisted with adjustment for numerous covariates and total protein intake. Conversely, no significant association with other sources of protein such as poultry, fish, eggs etc and ESRD could be found. This association of red meat and ESRD persists in separate analyses including non-ESRD CKD deaths (Table 4), patients with a minimum of 4 years follow-up (Supp Table 1 & 2) and patients without a history of diabetes, hypertension, coronary disease or stroke, which the authors argue could be conditions likely to co-occur with CKD (Supp Table 3).
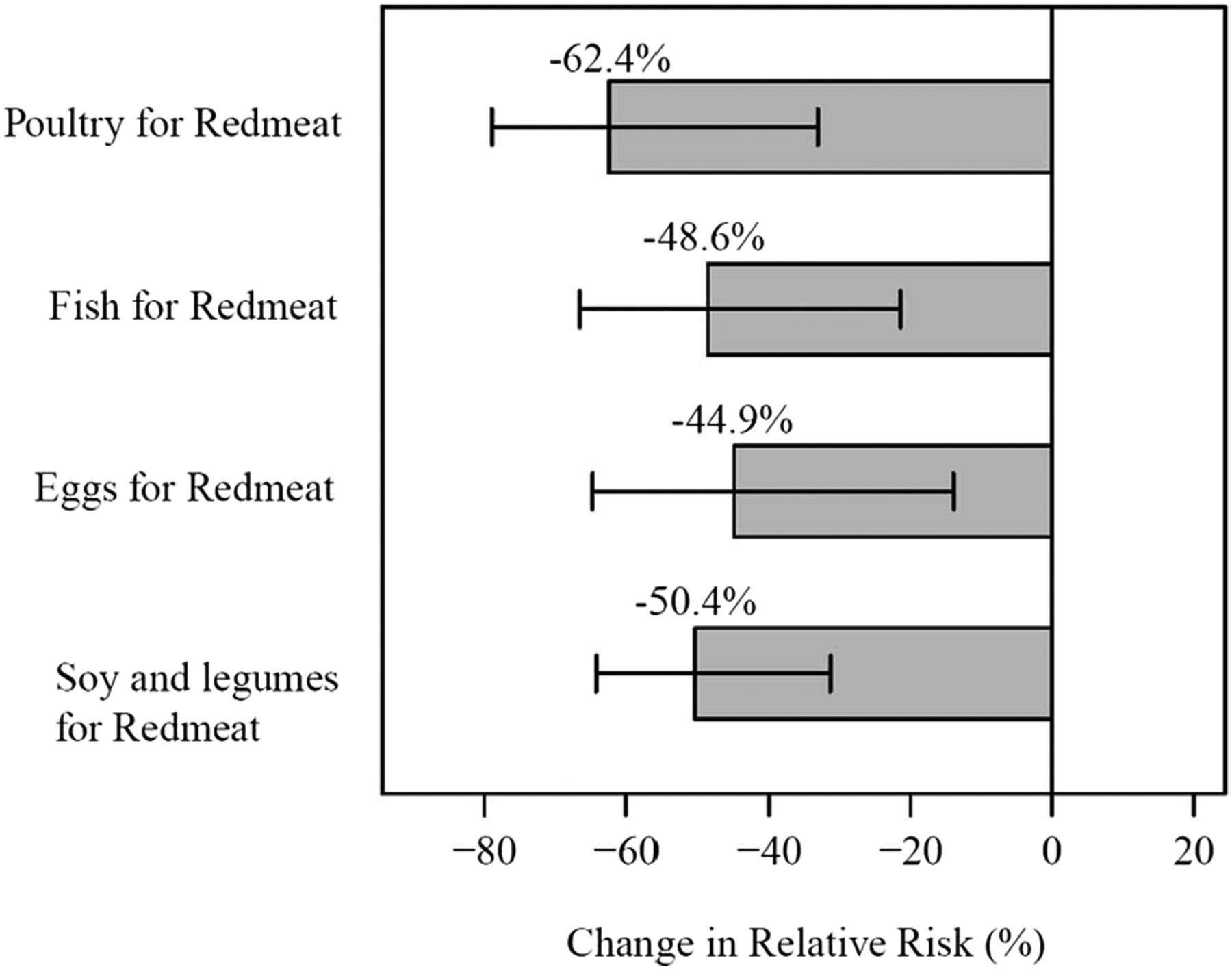
Finally, the authors use some statistical machinations to model a potential effect of substituting one serving of red meat with another source of protein (Figure 2). This produces relative risk reductions of between about 45 and 60% for ESRD depending on the substituted source of protein.
Figure 2 from Lew et al, JASN 2016
Substituting one serving of red meat with one serving of poultry, fish, eggs, or soy and legumes resulted in significant percent reduction in relative risk of ESRD; all P<0.01.
Discussion
So, where and how can we use this study? I will leave the debate for the chats, but can this study support red meat restriction in CKD patients to prevent disease progression? Does it even say anything about CKD at all? Or does it just tell me to skip that steak…