#NephJC chat
Tuesday Sep 6th 9 pm Eastern
Wednesday Sep 7th 8 pm BST; 12 noon Pacific
Effect of regional versus local anaesthesia on outcome after arteriovenous fistula creation: a randomised controlled trial
Aitken E, Jackson A, Kearns R, Steven M, Kinsella J, Clancy M, Macfarlane A.
PMID: 27492881
Clinical Trial Registration: NCT01706354
Introduction
Historically nephrology is a specialty that has been criticized for it’s inability to produce high quality, randomized controlled clinical trials designed to answer a specific question. So, when the Lancet publishes the results of a clinical trial in the field it is worth taking note.
Background
Most nephrologists will agree that for the majority of hemodialysis patients native AVF confers a significant survival advantage over tunneled dialysis catheters and grafts (though in selected elderly patients I acknowledge fistula first may not always be the best strategy). A large proportion of surgically created AVF fail to mature and are unable to be used as a dialysis access. This failure can occur at an early stage. Multiple factors contributing to the failure:
- pre-operative size of the arteries
- pre-operative size of the veins
- Blood flows within the vessels
- Early post-operative blood flow
It is this final point that appears most pertinent to this study, as early post-operative blood flow is a potentially modifiable factor to improve graft survival. General anesthesia obviously causes vasodilation that may be beneficial to early post-operative blood flow, but necessarily is associated with the risks of general anesthesia – particularly for patients with ESRD and advanced CKD. Regional and local anesthesia both avoid the risks of a general anesthetic, but regional brachial plexus blocks (BPB) result in additional regional sympathetic nerve blockade and arterial and venous vasodilation peri- and post-operatively.
This study tested the hypothesis that native AvF’s created under regional anesthesia would improve primary patency rates at three months.
Methods
This study was an observer blinded, RCT conducted across three large teaching hospitals in Glasgow, UK. It was conducted in adult patients (>18 years) who were having primary brachiocephalic or radiocephalic fistula formation. Patients who had previously had an ipsilateral fistula attempt or whose blood vessels were below a certain diameter (radial/brachial artery <1.8mm, cephalic vein <2mm at the wrist or <3mm at the elbow) were excluded. There were some other sensible exclusion criteria including central venous stenosis (even if treated).
Randomization was 1:1, BPB or local anesthetic. The evaluators were blinded but the surgeon performing the procedures not. Whilst there was no standardized operating protocol, all procedures were conducted by 1 of 9 experienced surgeons who followed a largely similar surgical technique. BPB was carried out under USS guidance by 1 of 2 senior anesthetists or senior trainees under supervision. Local anesthesia was administered by the operating surgeon.
126 patients (63 in each group) were enrolled based on a power calculation to detect an improvement in primary AvF patency at 3 months (the primary end-point) from 65% - 85% in the patients having BPB (80% power). Pre-specified secondary end-points included immediate patency, functional patency (assessed clinically or with USS) at 3 months as well as change in brachial artery blood flow and diameter and cephalic vein diameter immediately following administration of anesthesia and at 3 months.
Results
The study recruited the required number of patients (Figure: Trial Protocol)
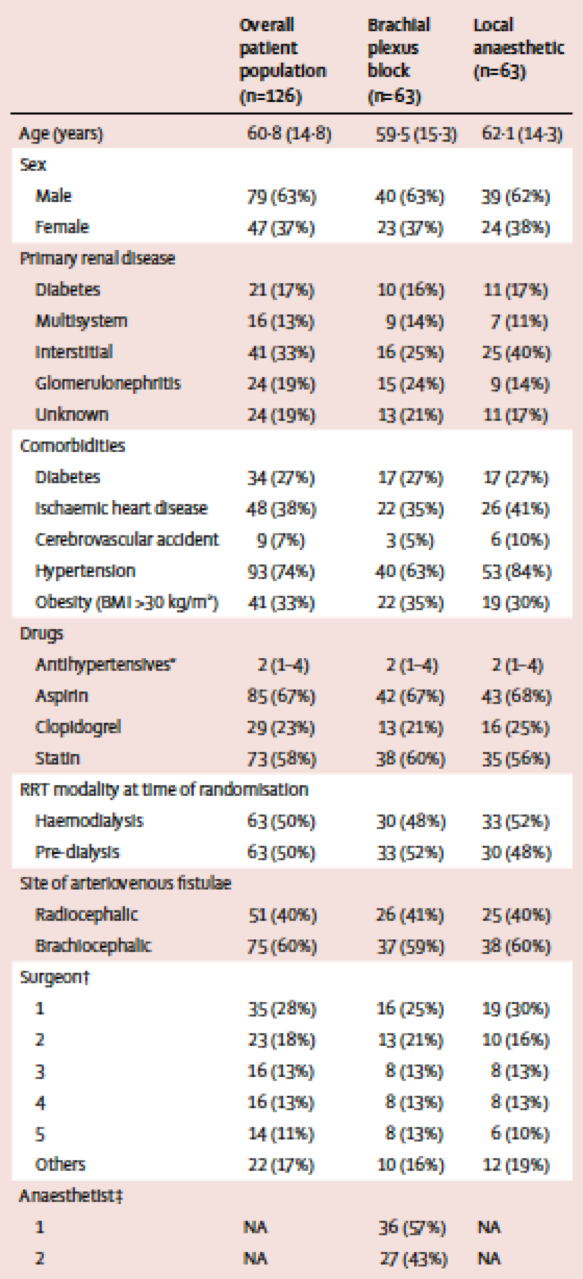
The groups were well managed in terms of demographics, operating surgeon, and site of access (Table 1) and looked very much like a representative sample of CKD/ESRD patients based on age and medical co-morbidity.
Table 1: Demographic and baseline details of both groups
Importantly there were no significant differences in the sizes or dimensions of any of the blood vessels between the groups. 40% patients had a radiocephalic fistula and 60% had a brachiocephalic fistula created.
The results for the primary outcome showed a significant improvement in primary patency at 3 months for patients who had their fistulae created under BPB compared to those whose fistulae were created under local anesthesia (84% vs 62%, odds ration 3.3, [95% confidence interval 1.4-7.6] p=0.005). Primary patency rates were increased for both radiocephalic and brachiocephalic fistulae, but were higher in the radiocephalic group (table 3). Similarly immediate patency rates were higher in the BPB group, and for radiocephalic fistulae rather than brachiocephalic fistulae (table 3). Functional patency at 3 months was not significantly different between BPB group and local anesthetic group overall, but was significantly better for patients who had radiocephalic fistulae (table 3).
It was also interesting to see that the diameters of blood all blood vessels increased at the time of anesthesia in the BPB group, and not in the local anaesthetic group, but at 3 months follow up, there was no difference between the size of the draining vein above the anastomosis.
Discussion
This is the first and currently only RCT on this issue and is therefore currently the best evidence we have for whether choice of anesthetic affects medium term fistula patency rates. This is undoubtedly a flagship paper, the question is whether this paper on it’s own is sufficient to alter practices immediately, or whether we need to wait for confirmatory studies with similar findings. I am (for once) going to keep my powder dry for the debate, but this is undoubtedly an important piece of research and the authors should be congratulated on their work.