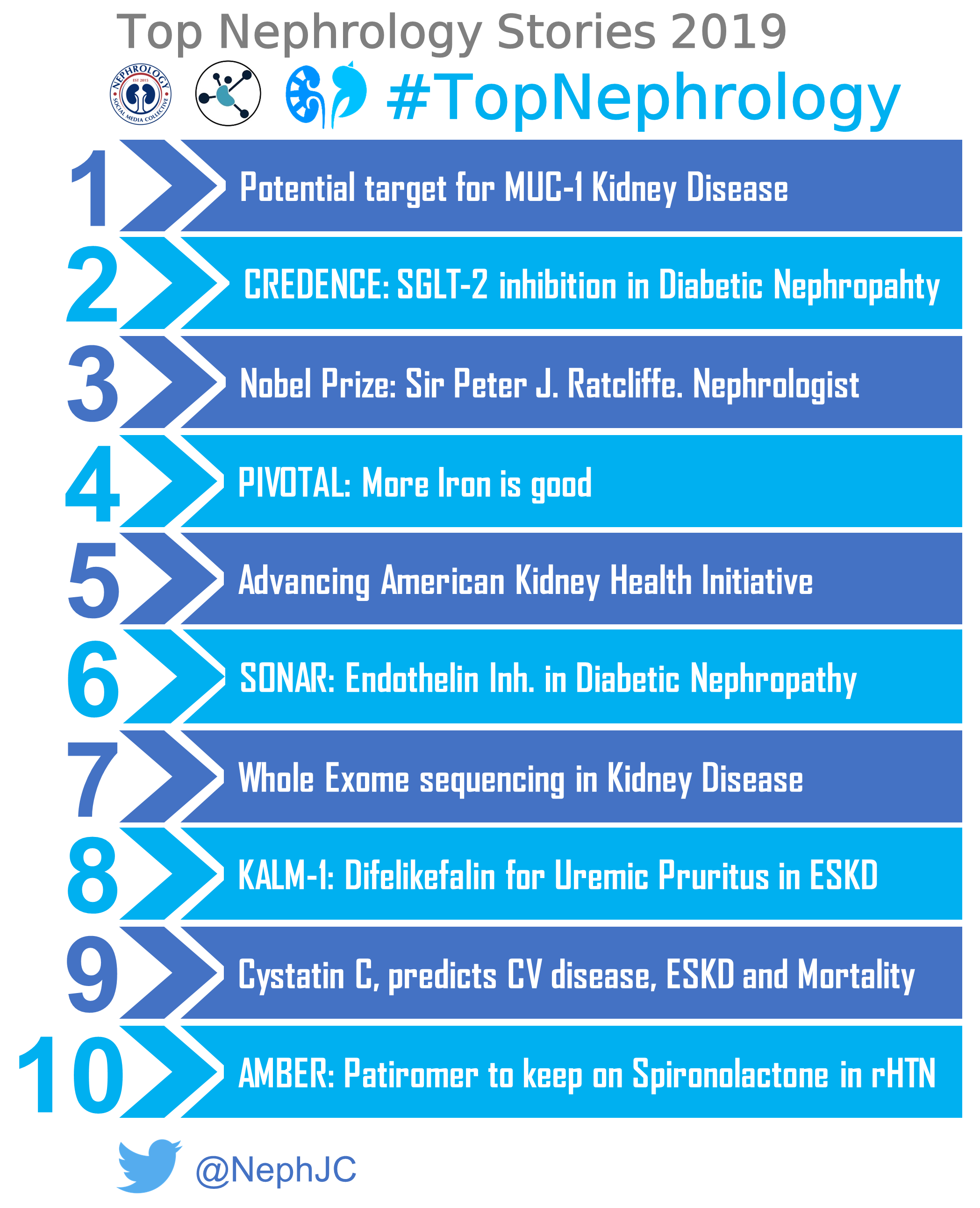
The votes are in and counted. NephJC proudly presents the Top Nephrology Related stories of 2019. Note- The MENTOR trial was not included in this years voting since it made the Top stories list of 2017 when it was originally presented.
10: Patiromer use to keep more on Spironolactone in Resistant HTN in Lancet
The new generation of potassium binders bind potassium but can they improve patient outcomes? Patiromer was studied in the AMBER trial in The Lancet to examine whether it allowed persistent use of spironolactone for treatment of resistant hypertension in CKD; in previous studies it enabled continuation of RAAS blockers by mitigating hyperkalemia (PEARL-HF, AMETHYST-DN, and OPAL-HK).
In this phase 2, randomized, double-blind, placebo-controlled trial, the primary efficacy outcome was met, with 86% patients receiving patiromer remaining on spironolactone at week 12 as opposed to 66% in the placebo arm; of note the study included patients with eGFRs as low as 25ml/min/1.73m2 (who had been excluded from previous trials). Whether patiromer will enable continuation of RAAS blockade where clinically indicated or whether it will be a practical intervention for patients remains to be seen.
9: Cystatin C predicts CV Disease, ESKD and Mortality in Nature Medicine
Cystatin C has been around for a long time. Although on paper it is an appealing marker of kidney function (freely filtered, not secreted, little is present in urine due to it being reabsorbed and catabolised in the proximal tubule), it is affected by non GFR factors including inflammation, diabetes and smoking. Its use is predominantly in research settings or in select clinical cases.
A study using the Cardiovascular Health Study cohort showed cystatin C was a strong and independent predictor of all cause of CV and all-cause mortality and was linearly associated with risk of death (creatinine and eGFR had a J-shaped association with risk of death).
Lees et al. study in Nature was a large prospective cohort study involving a UK BioBank; they showed eGFRcys is more strongly associated with future CVD events than eGFRcr for both CVD outcomes and future ESKD risk. eGFRcys identified a greater proportion of participants with CKD G3–5 than both eGFRcr and eGFRcr-cys.
To say adapting Cystatin C into clinical practice would require a paradigm shift in our practice would be an understatement. The benefit may be most pronounced in those not picked up by eGFRcr alone (eGFRcys 60-89 group which was associated with a 30% increased risk of mortality and CVD). This study highlights we need to rethink Cystatin C as a potential clinical marker in greater detail.
8: Difelikefalin for uremic pruritus in ESKD in NEJM
Difelikefalin is the first drug ever for the treatment of uremic pruritus. Think about that, we have never had a treatment for this common effect of kidney failure and, though not approved, there is now an effective treatment. The unpronounceable, difelkefalin had its moment in primetime during Kidney Week when Dr. Fishbane presented the phase three trial along with simultaneous publication in the NEJM. Difelkafalin is an IV (for now) Kappa agonist that cannot cross the blood brain barrier. It doesn’t have the addictive or euphoric properties usually associated with opioids and was able to meaningfully reduce the uremic pruritus for nearly half the cohort. It will be interesting to watch this drug go through the FDA New Drug Approval process in 2020.
7: Whole Exome Sequencing in Kidney Disease: Groopman et al in NEJM
Do you know the cause of chronic kidney disease for every patient you follow? Are you sure? You may start to question yourself after reading this powerhouse of a genetics study in the New England Journal of Medicine from Dr. Ali Gharavi’s lab at Columbia. First author Emily Groopman and colleagues performed whole exome sequencing on over 3000 patients with CKD and yielded a genetic diagnosis in almost 10%. Yield was even higher for patients with congenital or cystic kidney disease (23.9%) and nephropathy of unknown origin (17.1%). Type IV collagen mutations were the most frequently identified in the entire cohort, however 62% of these patients didn’t have a prior diagnosis of Alport syndrome and had been carried as the generic diagnosis of FSGS. Will whole exome sequencing become standard of care for all patients with CKD? We’re entering a new era of genetic diagnosis in nephrology.
6: Endothelin inhibition in Diabetic Nephropathy: SONAR in Lancet
The excitement around the CREDENCE overshadowed another important publication, that of the SONAR trial. Following on the previous RADAR trial (which was the second NephJC ever), the SONAR trial examined the benefit of atrasentan, which is an endothelin antagonist. This class of drugs has the nasty effect of causing sodium retention, as reported in the ASCEND trial a decade ago. To overcome these issues, the SONAR trial used an adaptive design (see this tweetorial for more links on the topic). The investigators chose patients with proteinuric diabetic nephropathy - who had significant proteinuria despite RAS blockade. In addition, they had to tolerate atrasentan in a run-in period - too much sodium retention (despite added diuretics which everyone had to be on) and they were out. In this ‘enrichment’ period, they also had to show a 30% proteinuria reduction. Partly as a result of these stringency, the enrolment came down from ~ 11,000 screened, to ~ 5000 entering the enrichment period, and finally 2648 actually entering the double blind RCT phase. Consequently, the sponsor pulled the plug on the trial since event accrual was slow. By the time all the numbers rolled in, however, there was a benefit in with atrasentan, with a hazard ratio of 0.65 for the composite renal endpoint. There were some very intriguing & plausible findings in the subgroup analysis as well, discussed in the Freely Filtered podcast. Atrasentan was lost in the noise, since the sponsor is not developing the molecule, but other promising trials continue (eg Sparsentan in glomerular diseases and Aprocitentan in resistant hypertension).
5: Advancing American Kidney Health Initiative
One of the most exciting happenings this year (and maybe the last several decades) was the signing of an executive order called the Advancing American Kidney Health Initiative on July 10th, 2019 in Washington DC. You can watch the announcement here. This executive order is geared at tackling three goals:
Prevent kidney failure through better diagnosis, treatment, and preventative care.
Increase affordable alternative treatment options, educate patients on treatment alternatives, and encourage the development of artificial kidneys.
Increase access to kidney transplants by modernizing the transplant system and updating counterproductive regulations.
The details of this executive order is still being worked out. The ASN Website has a lot more information that is continuously being updated. This is a very exciting initiative and frankly way overdue in the US. Once implemented the executive order has so much potential to really change the landscape of kidney disease in the US. Bravo. What a year 2019 was.
4: More Iron, more better. PIVOTAL in NEJM
Anemia in kidney disease is a story of medical reversals. Increasing hemoglobin with erythroproietin is good. Maybe not so good. Alright, it’s actually bad. But increasing hemoglobin with epo still increases quality of life. No, it actually doesn’t. Surely if increasing hemoglobin with epo is bad, increasing it with iron cannot be not good either? We know free iron can help in the development of free radicals and oxidant damage in tissues. Iron overload is also associated with septicemia and weird infections. Hence we follow the ferritins and hold iron and all the other shenanigans. The first hints that we were wrong about this is the DRIVE trial, which showed that giving more iron in patients with high ferritin and no signs of active infection was effective in increasing hemoglobin without any safety signal for cardiovascular or infectious risk. The PIVOTAL trial was the final nail in the rusty coffin of iron being a bad actor. This was a prospective investigators lead multicentre trial, of a proactive compared to a reactive iron strategy with mortality and MACE as primary outcome. In the proactive strategy, participants received 400 mg intravenous iron per month (with a safety cutoff somewhat arbitrarily set at 700 for ferritin and less arbitrarily at 40% for iron saturation). In the reactive strategy, the iron target was set at a ferritin of 200 and saturation of 20%. As one would expect, more iron meant less epo usage, higher hemoglobins, and less blood transfusions. But as one might not have expected, it also resulted in a 16% lower hazard for all cause mortality, with no safety signal whatsoever against giving more iron. Take the red pill, rather, open your mind and give the iron infusions. Ferritins don’t matter anymore (in the absence of infections, needless to say).
3: A Nephrologist Awarded the Nobel Prize: Sir Peter J. Ratcliffe
2019 was the year that a nephrologist won the Nobel Prize in Physiology or Medicine for the first time. Nobel Prizes have been won for other important nephrololgy related topics in the past, but never has a bona fide nephrologist taken the top prize. Sir Peter J Ratcliffe (Director for the Target Discovery Institute within the Nuffield Department of Medicine at Oxford University and Director of Clinical Research at Francis Crick Institute, London) along with William G Kaelin Jr from Harvard University and Gregg L Semenza of Johns Hopkins University won the prize for their discoveries about how cells sense and adapt to oxygen availability, particularly their work in understanding the role of hypoxia inducible factor (HIF) in oxygen sensing. These findings led to the development of a novel class of drugs to treat anemia due to chronic kidney disease, the HIF prolyl-hydroxylase inhibitors (vadadustat, roxadustat, daprodustat currently in clinical development). Can’t wait for the next nobel prize winning nephrologist!
2: SGLT2 inhibition in Diabetic Nephropathy: CREDENCE in NEJM
This is a story long awaited. We have known about the glucoretic activity of phlorizin, found in the bark of green apples (and trace amounts in the strawberry) for long - but this was not useful since phlorizin gets inactivated in the small intestine. Synthetic analogues - canaglifozin, empaglifozin, dapaglifozin, ertuglifozin with a couple more in various stages of development, have shown glucose lowering effect. In the last few years spurred by the FDA guidance, EMPAREG, CANVAS, and DECLARE-TIMI showed clear cardiovascular benefit with these agents. But the kidney is not the heart. Even the publication of the EMPAREG-Renal findings seemed to come as a surprise, since the kidney outcomes were not part of the prespecified primary or secondary outcomes. Wiser heads may have suggested otherwise, since we knew about the effects of SGLT inhibition on tubuloglomerular feedback. Fortunately, a team from Sydney put together the CREDENCE trial, with the nephrocentric primary outcome of ESKD, doubling of creatinine, or death. The rest, as they say, is history. CREDENCE lifted the dry spell of negativity which clouded the nephrology world for the last 2 decades. Read the trial, the NephJC summary, the chat wrapup, or listen to the podcast. Prescribe SGLT2 inhibitors and prevent kidney failure.
1: Potential Target for MUC-1 Kidney Disease in Cell
Advances in human genetics are making huge strides in our understanding of many diseases. It is impressive to see how we went from knowing little about inherited tubulointerstitial kidney diseases to now mapping out the mutated genes, defining the pathophysiology, to getting closer and closer to novel therapies. Medullary cystic kidney diseases have mapped to mutations in either MUC1 (Mucin-1) or UMOD (Uromodulin). Cracking the case of MUC1 kidney disease took some time because of the challenging sequencing that was required with the multiple variable number tandem repeats in the MUC1 gene. The mutation found in affected individuals results in a frameshift mutation, leading to a new truncated protein called MUC1-fs. The number 1 Nephrology-related story of the year in 2019 from Dvela-Levitt et al in Cell further describes the pathophysiology of MUC1 Kidney Disease and identifies a potential therapeutic molecule. The was all covered on NephJC and you can follow the story with this tweetorial as well. This truncated protein (MUC1-fs) is unable to be inserted into cytoplasm and accumulates and for some reason after many years triggers the unfolded protein response (UPR) leading to cell toxicity and eventually apoptosis. The group defined the reasons for this and identified a small molecule (BRD4780) that targets TMED9 and results in degradation of the toxic MUC1-fs. Further studies will need to be performed to see if treatment with BRD4780 results in improved kidney function in animal models and human studies will need to be performed next. Will look forward to seeing how the story “unfolds”.
Post written by Matt Sparks, Joel Topf, Michelle Rheault, Swapnil Hiremath, Laura Slattery
Infographic by Laura Slattery and Verner Venegas