#AskASN Chat
Tuesday Feb 21 2023 9 pm Eastern
Quality Assessment, Improvement and Education for Medical Directors of Dialysis Facilities
The ASN Excellence in Patient Care focuses on ASN’s clinical priorities to provide high-quality care for people with kidney diseases.
The EPC has three aims:
To ensure all people with kidney diseases receive the best evidence-based care possible.
To champion patient experiences, preferences, and values by actively engaging people with kidney diseases in EPC activities.
To dvance equitable access to high-quality kidney care by promoting diversity, equity, and inclusion and pursuing health care justice.
In this chat, NephJC collaborates with the ASN:EPC to discuss specific elements of education that are important for medical directors of dialysis facilities.
Medical Directors Have a Defined Job
The Centers for Medicare and Medicaid Services (CMS) mandates dialysis facility medical directors to play a major role in quality assessment, quality improvement and patient safety. Dialysis facilities can be made into high-reliability organizations, and leadership in those facilities should deploy continuous quality improvement techniques, use failure-mode effects analyses, and learn effective leadership strategies to accomplish better outcomes for dialysis patients.
Where to start
Quality improvement can start with measurement of evidence-based best practices, like those endorsed by the National Quality Forum. But why stop there? Quality improvement is enhanced by measures selected by patients and can be individually crafted to each patient’s needs and choices.
Safety Improvement
To maintain safety in the dialysis facility, attention should be directed to the source of many safety failures:
medication errors
infections
hyperkalemia
access-related problems
patient falls
Useful tools to prevent adverse events include root cause analysis, simulation exercises, human factors engineering and patient observation and participation in safety activities.
Infection Prevention
Infections are the second leading cause of death for dialysis patients, accounting for more than 10% of deaths in the US.
Medical directors can reduce these life-threatening infections with the following strategies:
effective patient and staff education
human factors analysis to better match staff with work responsibilities
effective leadership education.
Dialysis rounds that add infection prevention metrics to the usual quality measures (ex., anemia, bone disease, BP control) can reduce risk.
What about our nephrologists-in-training?
There’s something for them, too!
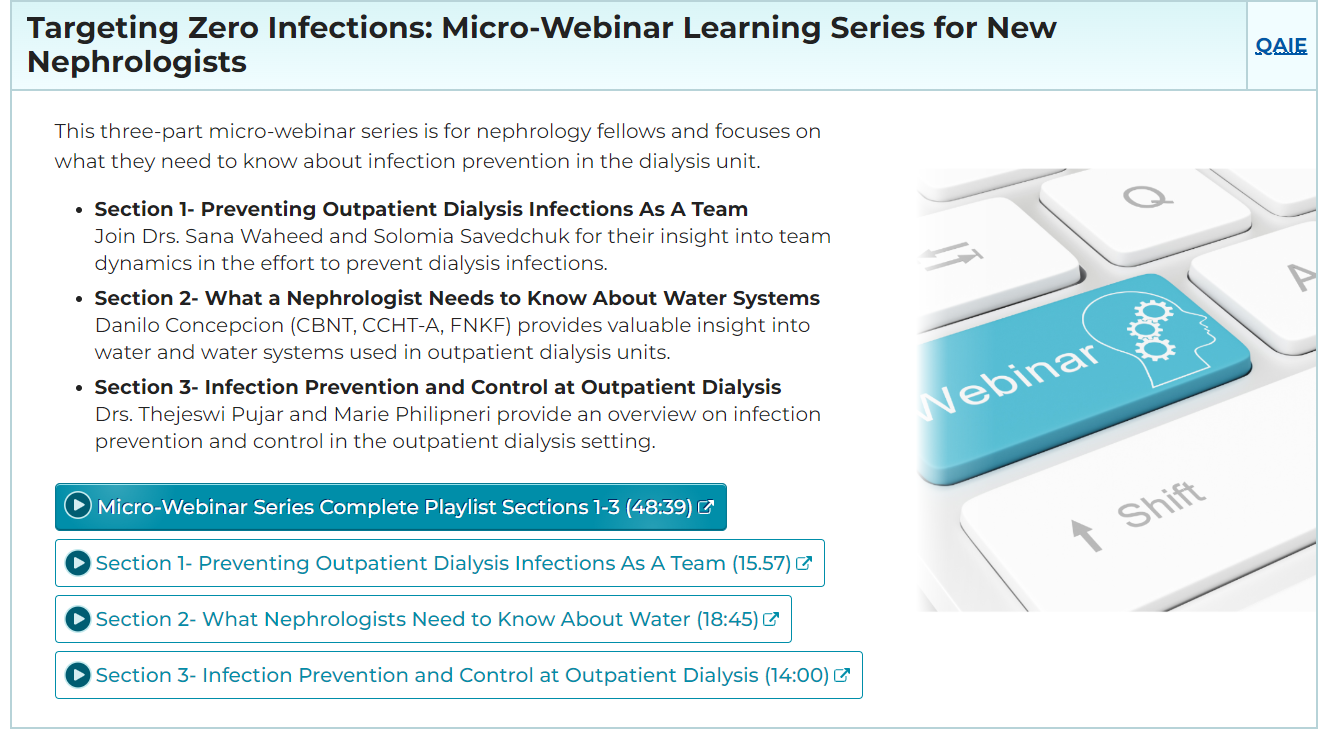
The ASN has prepared a new micro-webinar series for fellows. This focuses on what they need to know about infection prevention in the dialysis unit.
With all these resources and the community behind us, we can make the dialysis unit a safer and more effective place.
Summary prepared by
Alan Kliger, MD
Chair of the ASN Excellence in Patient Care
Advisory Committee