#NephJC Chat
Tuesday, December 5, 9 pm Eastern
Wednesday December 6, 8 pm GMT, 12 noon Pacific
J Clin Invest. 2017 Sep 1;127(9):3367-3374. doi: 10.1172/JCI89812. Epub 2017 Aug 7.
Phenotypic and pharmacogenetic evaluation of patients with thiazide-induced hyponatremia.
Ware JS, Wain LV, Channavajjhala SK, Jackson VE, Edwards E, Lu R, Siew K, Jia W, Shrine N, Kinnear S, Jalland M, Henry AP, Clayton J, O'Shaughnessy KM, Tobin MD, Schuster VL, Cook S, Hall IP, Glover M
PMID: 28783044 Full text at JCI
Introduction
Thiazide and thiazide-like diuretics are recommended as first line therapy for essential hypertension due to their significant morbidity and mortality benefit found in major RCTs including ALLHAT and SHEP. However, these medications can have unfavorable metabolic side effects including hyponatremia, hypokalemia, hypomagnesemia, hyperglycemia, hyperlipidemia, hyperuricemia. Of these, the mechanism of thiazide induced hyponatremia (TIH) is poorly understood. TIH occur in up to 15% of treated adults and is one of the most common causes of severe hyponatremia in adults. Interestingly TIH is reproducible with drug re-challenge in some patients (the hyponatremia can be induced with a single dose in susceptible patients). The elderly are particularly susceptible.
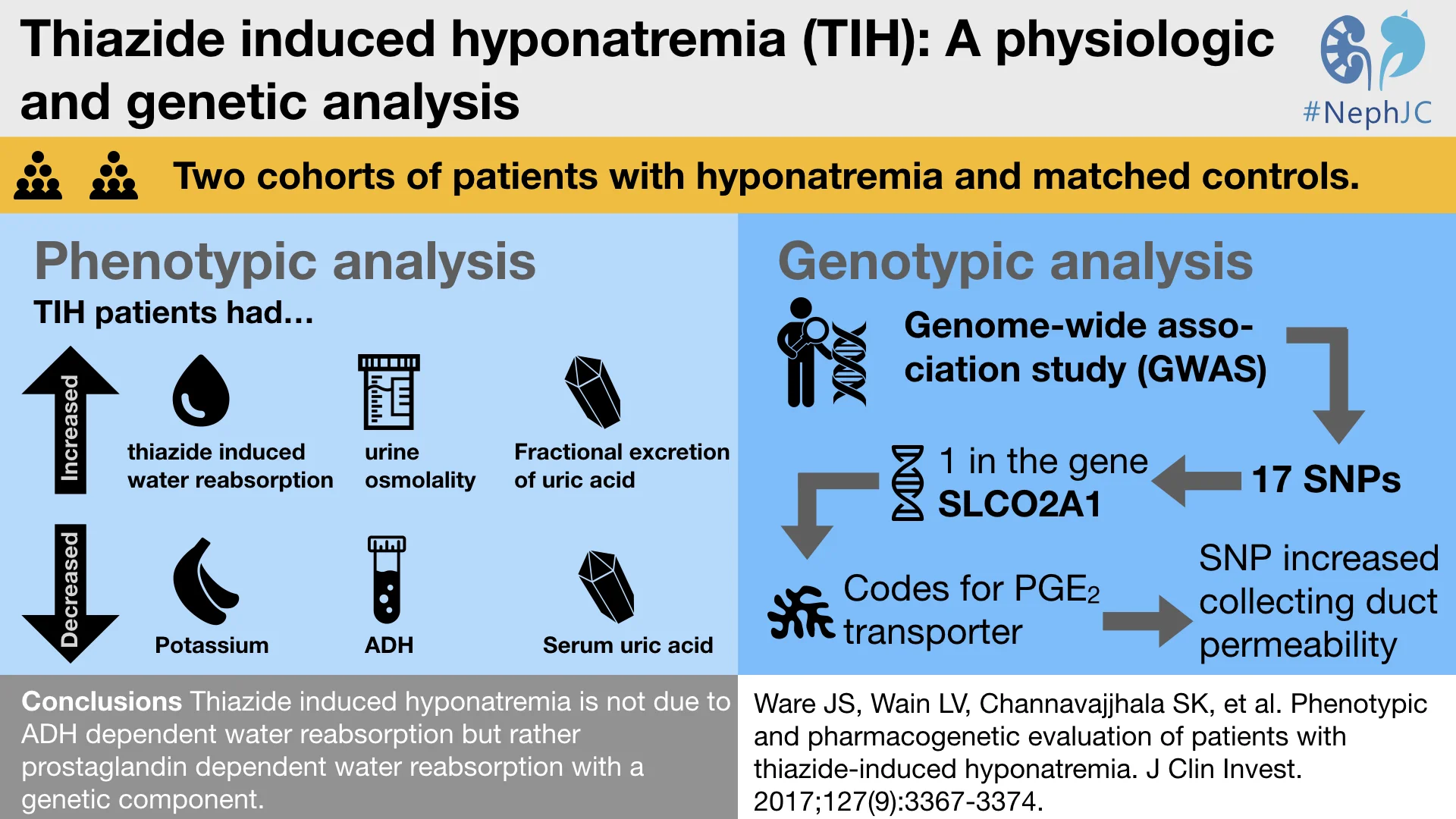
Dr. James Ware and colleagues conducted a comprehensive phenotypic analysis and genome wide association study (GWAS) of two cohorts of patients with TIH. Further validation of the candidate gene SLCO2A1 encoding the prostaglandin transporter (PGT) was studied using protein staining of human kidney tissue by immunofluorescence and in vitro assessment of gene variants of protein function.
Methods
TIH patients were identified from a daily EMR search of all medicine patients admitted to Nottingham University Hospitals NHS Trust.
Cohort 1 was enrolled from 2002-2003 and included matched normonatremic controls on thiazides from primary care clinic.
Cohort 2 was enrolled from 2012-2015 and included a more comprehensive phenotypic analysis. These patients had a 2 month follow-up evaluation after discontinuation of the thiazide diuretic when they were normonatremic. This cohort also included normonatremic thiazide controls and normonatremic non-thiazide controls.
Inclusion criteria:
Serum sodium <130 mEq/L
Late teens to 100 years of age
Thiazide or thiazide-like diuretic
IV fluids had not been administered
Exclusion criteria:
Advanced kidney, liver, or heart disease
Pregnancy
SIADH
Untreated endocrine disease
GI losses
Glucose >250 mg/dL
Clofibrate, carbamazepine, chlorpropamide, anti-neoplastics
Any other identified cause of hyponatremia
Results
GWAS
17 single nucleotide polymorphisms in 14 regions were identified that were significantly different in TIH compared to the general population controls (P < 10^-5). From these, SLCO2A1, rs34550074, p.A396T, was identified as a SNP of interest due to its high expression in kidney tissue and its role in renal salt and water handling. The protein product of SLCO2A1 is the prostaglandin transporter (PGT),
54% of TIH cases carried at least 1 copy of the variant allele
25% of controls carried at least 1 copy of the variant allele
Phenotypic analysis
The average age was late 70s to 80 years of age and both cohorts were mostly women. Bendroflumethazide was the most frequently used thiazide diuretic. 10% or less of patients were taking an SSRI and less than 6% of patients were taking NSAIDs
Cohort 1
The mean serum sodium from cohort 1 was 118 mEq/L compared to 139 mEq/L in the control group.
Cohort 2
Hyponatremic TIH patients had higher plasma renin and aldosterone compared to when they were normonatremic. However, hyponatremic TIH patients had the lowest serum and urine uric acid concentrations but the highest fractional uric acid clearance suggestive of volume expansion. Surprisingly, hyponatremic TIH patients were 0.8 kg heavier during hyponatremia than during normonatremia, suggestive of water retention [Ed. Remind me again why thiazide induced hyponatremia is categorized as volume depletion hyponatremia?].
TIH patients during normonatremia still had a lower mean serum osmolarity compared to both control groups (288 mosmol/kg compared to 295 mosmol/kg and 293 mosmol/kg). TIH patients had lower 24-hour urine osmolality during hyponatremia and normonatremia than the control groups. TIH cases reabsorbed 48% more free water when on thiazides compared with when off thiazides while controls had only a 9% increase in free water reabsorption while on thiazide. Solute free water reabsorption was lower in hyponatremic TIH cases on thiazide than normonatremic thiazide controls. Unexpectedly and despite these findings, hyponatremic TIH cases on thiazides had the lowest mean plasma ADH among all groups!
Yeah, we can't explain it either.
TIH patients had an increased 24-hour urinary prostaglandin E2 (PGE2) and PGE2 metabolite (PGE2-M) in response to thiazides. Furthermore, patients with the SLCO2A1 p.396T (variant) allele had higher urinary PGE2 and PGE2-M during both hyponatremia on thiazide and normonatremia off thiazide than the p.396A (wild type) allele.
Immunofluorescence of normal banked kidney tissue localized PGT to the proximal straight tubule, outer medullary collecting duct, and was most abundant in the inner medullary collecting duct.
Discussion
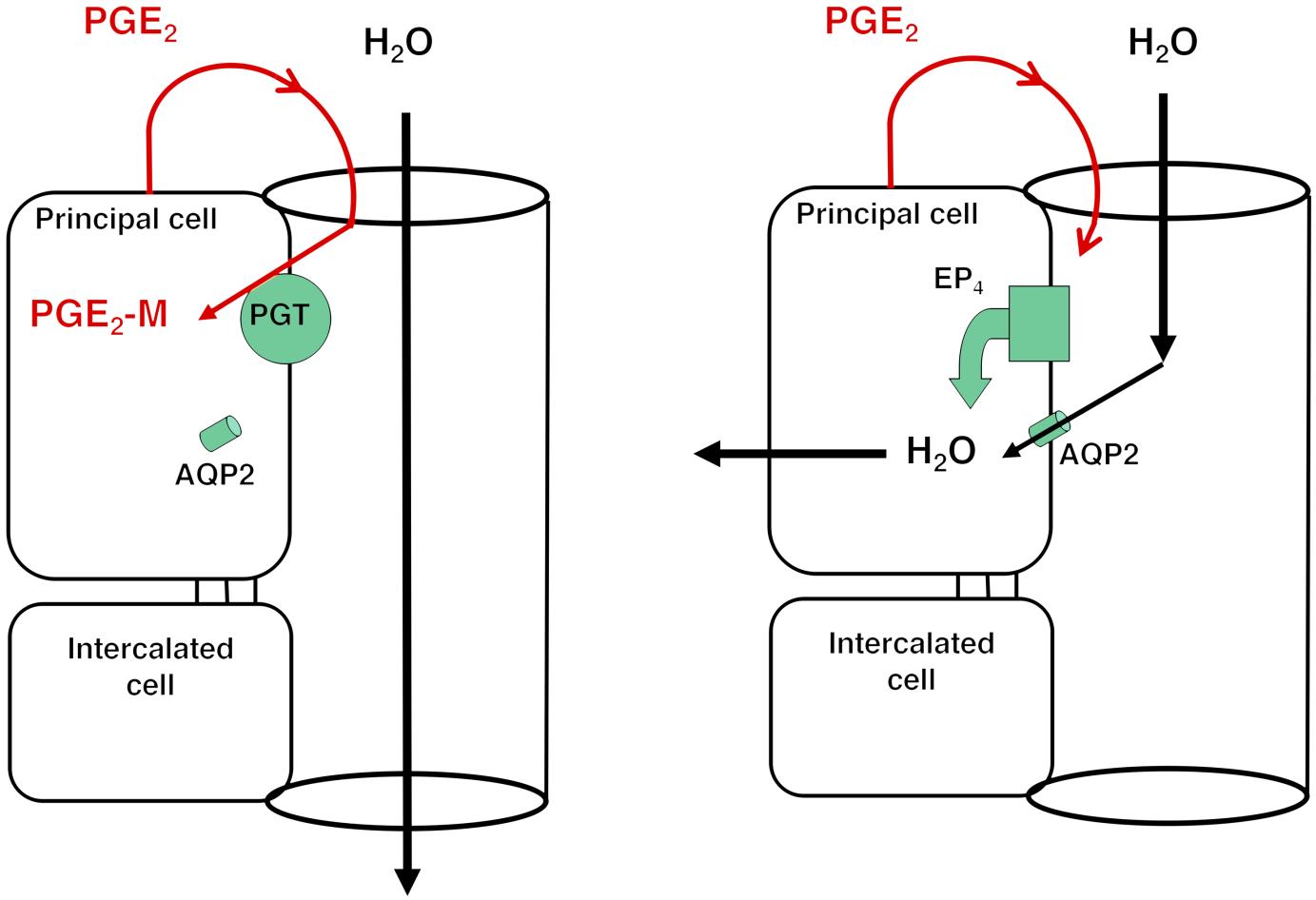
This study is the largest and most detailed study of TIH and provides insight into how they may cause altered water handling. The investigators conducted a detailed analysis of the TIH phenotype using blood, urine, genomic analysis, and tissue analysis. They used this to create a novel model of TIH. They theorized that reduced PGT activity in patients with the SNP increases collecting duct water permeability from luminal PGE2 increasing apical AQP2 abundance and activity.
LEFT: Under low ADH conditions, apical PGT in the renal collecting duct scavenges PGE2 from the lumen, resulting in AQP2 internalization and minimal osmotic water reabsorption.
RIGHT: With reduced or absent apical PGT, PGE2 reaching the lumen is able to stimulate apical EP4 receptors, resulting in insertion of AQP2 and osmotic water reabsorption.
However, the study has several limitations:
The single center design with patients of mixed European descent.
The study design did not allow for the determination of duration from first thiazide dose to hospitalization.
Immunofluorescence was performed in tissue obtained presumably from normonatremics rather than hyponatremics. Staining showed whole cell PGT staining rather than localizing to the apical or basolateral membrane.
An editorial by Hoorn and Wetzels mentioned the following criticisms:
FEUrate is an inaccurate measure of volume status and a higher BUN, creatinine, renin, and aldosterone during thiazide therapy supports volume contraction.
Assuming normonatremia reflects baseline serum sodium, a decrease in sodium from 137 to 122 and an increase in body weight from 65.5kg to 66.3kg does not fully support the hyponatremia is solely from water retention. This degree of decrease in serum sodium would require a weight gain of ~2.5-3kg.
Lastly, we are left with many questions:
How does a gene variant contribute to the phenotype typically seen in elderly women?
What about the other ~50% of the cohort without the SNP in PGT?
Could the SLCO2A1 polymorphism be relevant in other forms of hyponatremia such as SIADH?
Does the PGT mutation have a role in the hypothalamus/posterior pituitary?
Joshua Rein, DO (@ThepHunClub), Nephrologist,
Icahn School of Medicine at Mount Sinai, New York