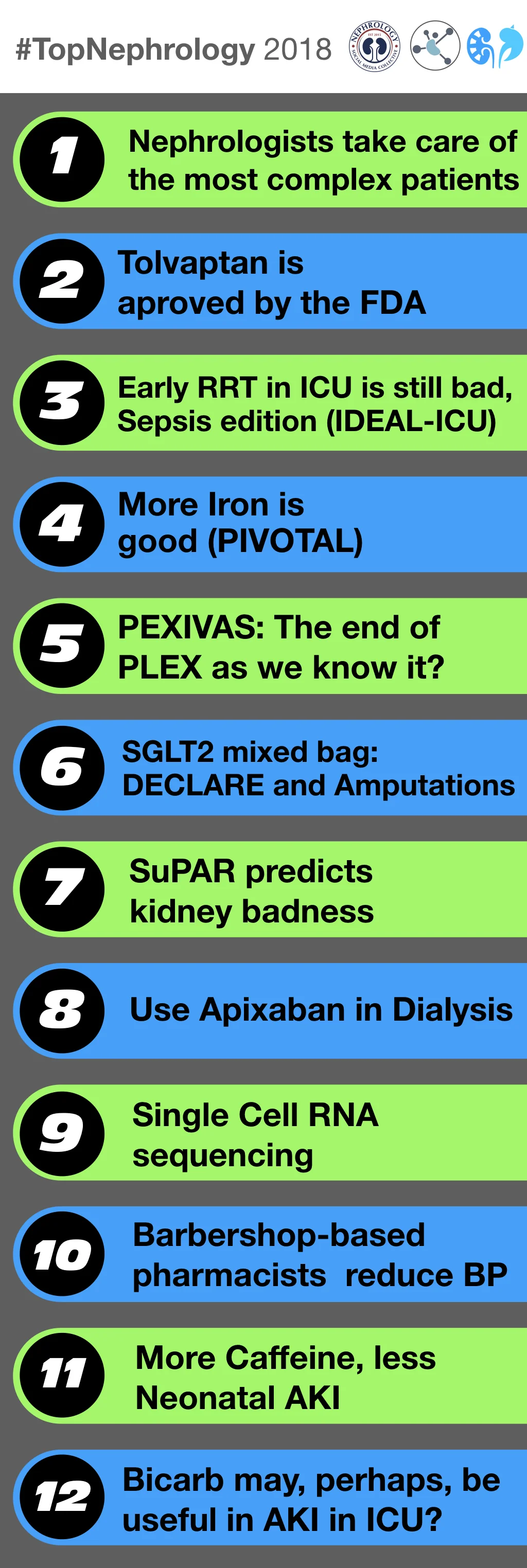
The people of NephTwitter have spoken. Without much ado, here are the top nephrology stories of 2018.
12: Bicarb may, perhaps, be useful in AKI, in the ICU
The reason many nephrologists choose nephrology is they love to fix the numbers. The unfortunate truth though, is that little of that number fixing is supported by rigorous evidence. One of the most controversial electrolytes to correct is bicarbonate in metabolic acidosis. There is plenty scientific rationale for using alkali to correct the acidemia but an equal amount of arguments against correcting it. But the rubber meets the road in clinical trials and in the summer of 2018, the Lancet published the largest study to date on the use of sodium bicarbonate to correct metabolic acidosis in the ICU. The top line results was no improvement in the primary outcome (organ failure at day 7 and any cause of death day 28). A more subtle read revealed that the pre-determined subgroup of AKI (AKIN 2 or 3) did benefit from the intervention. So the study provided ammunition for both sides. See the discussion on NephJC by Nimra Sarfaraz and the visual abstract by Divya Bajpai.
11: More caffeine, less neonatal AKI
Acute kidney injury (AKI) is common in children born prematurely with an incidence of up to 30% according to the recent multicenter Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) study. AKI in neonates is not just a lab anomaly, but is associated with a 4-5x higher odds of mortality in affected children and possibly increased risk of future CKD. In our number 11 spot for #TopNephrology stories of the year is a fascinating secondary analysis of the AWAKEN data that found an association between early caffeine administration and decreased risk of acute kidney injury in premature neonates in the first 7 days of life (adjusted odds ratio 0.20, 95% CI, 0.11-0.34). How on earth could caffeine prevent AKI and should I be giving it to everyone? Potential kidney protective effects of caffeine previously shown in animal models include increased renal blood flow and attenuation of oxidative stress. However, caffeine has also been associated with decreased incidence of sepsis, intraventricular hemorrhage, and bronchopulmonary dysplasia as well as reduced duration of mechanical ventilation in neonates, therefore reduced AKI may simply be due to reduced overall morbidity. Clearly, this is a topic that is crying out for further prospective studies. Without a Big Pharma backer for this inexpensive old drug, multicenter studies will rely on non-industry funding. The Neonatal Kidney Collaborative is organized and in an excellent position to successfully complete these and I expect to see them in the Number 1 #TopNephrology slot in the coming years.
10: Barbershop-based pharmacists reduce blood pressure
Coming in at 10 is the barbershop trial which was also the NephJC Kidneys study of the year. It has the perfect combination: a vulnerable and high risk population which is hard to reach and a novel intervention leveraging the primacy of barbershops. The additional aspect was the presence of pharmacists who could prescribe BP lowering medications. A fantastic reduction of just over 20 mmHg ensued. There are the naysayers who will nitpick. But the beauty of the barbershop trial is about effectiveness. We know how to reduce BP. But how do we reach the African American men who don’t go to the doctor? A lifelong program of study from the late Dr Ron Victor finally was vindicated. Check out the NephJC discussion and the visual abstract from Michelle Lim.
9: Single Cell RNA Sequencing
Coming in at number 9 is single cell RNA sequencing. NephJC highlighted two papers this year utilizing this technology. One in Cell Stem Cell from Wu et al and the other in Science from Park et al. So, what is going on here. Why all the fuss about RNA. The biggest advance single cell RNA sequencing (seq) allows is for a comprehensive unbiased approach to examining cellular alterations. Bias ruins all. Repeat (bias ruins all). The advent of RNA seq was huge. Before this, researchers hand picked genes to assay (single, multi, or in array). This led to a narrow window of observations and often times excluded potential game changing findings.RNA seq takes all available mRNA transcripts and quantifies them. Thus, giving you a complete picture of ALL alterations in transcribed genes. However, old school RNA seq had a problem. It took the tissue sample of many cell types and mixed them all up. Thus, you had no idea what cell was giving you the signal. Adding single cell RNA seq technology takes it to another level. Now to have resolution down to the level of each individual cell allowing for findings never seen before. The paper by Wu et al demonstrated that oranoid cellular differentiation differs by protocol used to produce them. The organoids also show to be fairly immature phenotype compared to the adult kidney. They also found that organoids grow neuronal cell clusters that can be reduced by inhibiting (with a NTRK2 inhibitor). Park et al. showed that many disease associated genes are expressed in single cells. Park et al. also found a novel cell type that express both principal and intercalated cell markers that is driven by the NOTCH pathway. How this technology continues to be applied will be very interesting. We predict it will continue to make impressive waves.
See the excellent summary and video summary by Jennie Lin or the visual abstracts from Sinead Stoneman.
8. Use Apixaban in Dialysis
How should we treat atrial fibrillation in dialysis patients? Atrial fibrillation is associated with higher stroke and mortality in this population. But give warfarin and bleeding rates, even major bleeds, go up. Enter the direct oral anticoagulants (DOACs), of which the most promising is apixaban. Though all the major trials excluded severe CKD and dialysis patients, some intriguing pharmacokinetic studies suggest 2.5 mg bid to be the ‘goldilocks’ dose. But a large observational study in the Circulation suggests otherwise. 5 mg bid was associated with lower event rates. And if you go back to the aforementioned PK study, you may see a hint of this if you squint closely at figure 1. Check out the NephJC coverage and the visual abstract from Sarah Gleeson. A proper trial is needed. Like yesterday.
7: SuPAR predicts Kidney badness
suPAR is to #TopNephrology countdowns as Vertigo is to “Best Movies Ever” lists; it’s always there.
I like to think of suPAR as nephrology’s Odysseus. Many of us probably first met our doughty hero during his exertions in the Trojan War, establishing various lines of evidence that he might be the permeability factor in FSGS. But since then, his wandering return to Ithaca has taken in many fresh tales and challenges. Whereas Odysseus travelled to the underworld, met Cyclops, the Lotus Eaters, and Circe, skirted the land of the Sirens and passed between Scylla and Charybdis, suPAR has been associated with incident CKD, and a declining eGFR, predicted CKD in African Americans regardless of APOL1 genotype, predicted mortality in African Americans with T2DM, and mortality in dialysis patients, and finally been suggested as a better marker of infection than CRP in AKI.
So will 2019 see suPAR return to slay the suitors to the permeability factor crown? I am not sure but no doubt you’ll be able to read all about suPAR in #TopNephrology 2019.
6. SGLT2i: Sweet or Sour?
Sweet pees are made of these...went the refrain from nephrologists fascinated by the glucoretic and natriuretic class of drugs, the SGLT2 inhibitors. First came EMPAREG, and last year was CANVAS, and now DECLARE reported that dapaglifozin reduced a composite outcome (mostly driven by heart failure). The benefit with dapaglifozin seemed less than with the other two - but this was a lower risk population; an accompanying meta-analysis of the three trials also did not report any such interaction. So can we declare mission accomplished and add these to the drinking water of diabetic households? The amputation signal seen in CANVAS is now reiterated in a large observational dataset. This dataset did not report any difference between the three drugs, giving us pause before we reach for the pen to prescribe SGLT2i (and a separate matter of whether nephrologists and cardiologists should be prescribing these drugs?) The SGLT2i story is slowly unfolding, and conclusions should be cautiously drawn. Many more trials are to come, with CREDENCE up next at the World Congress of Nephrology in Melbourne. Stay tuned.
5: PEXIVAS slays Plasmapheresis
Does your patient have ANCA vasculitis with severe kidney involvement and/or pulmonary haemorrhage? Then chances are you’re offering them plasma exchange and a treatment regimen with high dose steroids. The Pexivas trial, which was presented at a number of nephrology conferences in 2018 but as of writing, remains unpublished, may have news for you.
Presented results suggested firstly that plasma exchange does not affect the composite outcome of death or progression to end stage kidney failure in severe AAV, and secondly that a reduced dose steroid regimen was non-inferior to a standard protocol. The trial randomised 702 participants, and no pre-specified subgroup including age, ANCA type and serum creatinine showed a significant interaction.
As you can imagine, discussion of these data has been intense and no doubt will be reignited when the paper is published. For now remember the clinical trialists law: “Where a trial casts doubt on the efficacy of a treatment, the number of people calling for subgroup studies and meta-analyses of relevant trial results is directly proportional to the length of time people have been using this treatment, and how strongly they “know” it to work…”
4: More Iron is PIVOTAL
One of the biggest stages at Kidney Week is the late breaking and high impact trials. The only thing better than presenting during that session is presenting along with simultaneous publication in the NEJM. PIVOTAL did this at the 2018 Kidney Week meeting in San Diego. PIVOTAL is an etension of the work by Daniel Coyne’s DRIVE 2 trial which showed that additional iron despite high ferritin was both safe and effective (at raising the hemoglobin). Iain Macdougall and friends came up with an aggressive iron protocol and compared it to a reactive protocol:
high-dose iron sucrose, 400 mg monthly, unless the ferritin was >700 μg per liter or the transferrin saturation was ≥40% versus
low-dose iron sucrose, 0 to 400 mg monthly, only when the ferritin <200 μg per liter or a transferrin saturation of <20%.
The primary outcome was a composite of nonfatal myocardial infarction, nonfatal stroke, hospitalization for heart failure, or death. The study met its non-inferiority primary outcome. Importantly, while not reducing the primary outcome, it did reveal a number of intriguing secondary outcomes:
Reduced ESA dose 19%
Reduced transfusion rate 21%
No increased risk of infection or hospitalization
Reduced risk of hospitalization for heart failure
Reduced risk for recurrent events
Look for PIVOTAL to be discussed at NephJC sometime in 2019. In the meantime, read it in the NEJM.
3: IDEAL ICU: The end of early dialysis for AKI?
What’s the ideal time to start dialysis when a critically ill patient has AKI? The two big studies so far have reported mixed results, covered on NephJC a couple of years ago. More importantly, could critically ill patients with sepsis be different, given that they are sicker, so if there is any benefit, one would see it in these patients? IDEAL-ICU aimed to do what IDEAL did for timing of RRT in CKD. A multicentre trial from France, with almost 500 patients enrolled, this was stopped early for futility after it became clear there was no difference. Check out the twitter moment with more details. Divya Bajpai made an excellent visual abstract, for the last month blog post. We are not done, as an ongoing trial, STARRT-AKI (larger than all these three put together) is hitting its enrolment target, with over 2000 patients randomized so far. This question is so important, we are are sure to see it again on #TopNephrology in 2020, or perhaps even earlier, depending on the timing.
2: Tolvaptan approved for Polycystic Kidney Disease
Number 1 story in 2012: TEMPO 3:4, tolvaptan slows cyst growth (and loss of eGFR) in autosomal dominant polycystic kidney disease.
Number 6 story in 2013: Tolvaptan fails to get FDA approval for the treatment of ADPKD.
Number 8 story in 2015: Tolvaptan in UK and Canada gets approval
Number 4 story in 2017: Tolvaptan works again in the Reprise trial
Number 2 story in 2018: Tolvaptan (finally) gets FDA approval for the treatment of ADPKD. It has been a long road to get this drug available, but we now have something to offer patients with ADPKD besides blood pressure control.
1: Nephrologists Rock
It is perhaps no surprise that a paper telling us that nephrologists look after the most complicated patients is 2018’s #TopNephrology story. Not only does it give us a warm glow of affirmation, but also the idea itself feels a little like a “best of 2018” list, to be enjoyed and gently debated over a coffee or a drink.
The authors looked at about 2.6 million Canadians, 13 types of medical specialist, and 9 markers of patient complexity. These markers fell into 3 categories: 5 were raw numbers - comorbidities, types of physician seen, individual physicians involved in care, prescribed medicines, ED visits. 3 were rates – death, hospitalisation, and placement in long-term care. The 9th looked for presence of a mental health diagnosis. Interestingly, although nephrology came out top overall, it was ranked first in only 4 of 9 categories (comorbidities, prescribed medicines, long-term care placement, and mortality risk), with infectious disease topping the other 5.
The backlash from general/family practitioners/geriatricians/oncologists/any medically qualified person with a twitter account was swift, predictable and often very reasonable. For example, surely nephrologists taking care of patients with CKD5 on dialysis or with transplants confounded the whole thing? Yes, probably. But to be honest, I wasn’t too bothered about the details. Nephrology is hard: treating a young woman with SRNS, navigating a safe passage through an attritional decline in the health of an elderly man on dialysis, or supporting a newly transplanted patient through some unexpected difficulties. Recognition of this complexity is important. It strengthens me to keep nurturing long-term relationships with my patients and colleagues, and to keep going in the best specialty there is. See you in 2019. #NephForward