#NephJC Chat
Tuesday December 29 at 9 pm Eastern
Wednesday December 30, 2020 at 9 pm Indian Standard Time
Wednesday December 30, 2020 at 9 pm GMT
Kidney International Reports. https://doi.org/10.1016/j.ekir.2020.10.005
Safety of Remdesivir in Patients with Acute Kidney Injury or CKD
Sayali Thakare, Chintan Gandhi, Tulsi Modi, Sreyashi Bose, Satarupa Deb, Nikhil Saxena, Abhinav Katyal, Ankita Patil, Sunil Patil, Atim Pajai Divya Bajpai, Tukaram Jamale
Open AccessPublished: October 10, 2020
PMID 33073066
Other papers of interest:
Introduction
We now have the vaccine, or rather vaccines, with more to come. So is this topic still important? Unfortunately, the answer is yes. It is going to take many more months, or even perhaps years until the vast majority of humanity is vaccinated. In the interim period, the better we are at treating Covid, the more lives that will be saved. Clichéd but true.
The dearth of postulated therapies for Covid is impressive, particularly when we consider the timeline we are dealing with. Many therapies for Covid have fallen out of favour, especially after being tested in randomized controlled trials (RCTs). Steroids in the form of dexamethasone are now appropriately entrenched in any therapeutic regimen, especially for sicker patients needing oxygen.
Remdesivir (brand name Veklury, Gilead Inc) continues to enjoy popularity. Remdesivir is a prodrug that, after being metabolized to remdesivir triphosphate, acts as an analog of ATP, competing for incorporation by viral RNA-dependent RNA polymerase and thus interfering with viral RNA replication (see figure).
Mechanism of action for remdesivir. Figure from Adamsick et al, JASN 2020
Before we dive into the subject of discussion today, let us briefly consider what Remdesivir achieves. It received an emergency use approval (EUA) from the US FDA in May 2020, and soon after also from the European Medical Agency. For certain countries (India, Pakistan and Egypt), Gilead signed non-exclusive voluntary licensing agreements with generic pharmaceutical manufacturers to further expand supply of remdesivir for specific low middle income countries (LMICs, see full list of countries here).
The data for remdesivir efficacy comes mainly from the NIH lead ACTT and subsequently the more pragmatic WHO SOLIDARITY trials. With respect to mortality, there seems to be little effect, but it possibly has some benefit early in the course to shorten the hospitalization stay. At most.
The meta-analysis above shows the effect of remdesivir on mortality. With nicer mortality, and more granularity, you can see a published version below:
Figure from the WHO SOLIDARITY team, NEJM 2020
If you look closely at all the aforementioned RCTs, a common exclusion criteria was anyone with AKI or severe CKD, usually defined as a GFR less than 30. Why would that be an exclusion criteria? Is this drug nephrotoxic, does it accumulate in patients with reduced kidney function? The truth of the matter is that none of the above are true.
Of note, due to its limited water solubility. remdesivir requires to be administered with an excipient sulfobutylether-b-cyclodextrin (SBECD) . An excipient is a substance formulated alongside the active ingredient of a medication included for the purpose of long-term stabilization, bulking up solid formulations, or to confer a therapeutic enhancement on the active ingredient, such as facilitating drug absorption, reducing viscosity, or enhancing solubility. SBECD accumulates with reduced kidney function. Additionally, if it does accumulate, it can cause kidney injury. Apparently, this has been noted when it is used with voriconazole. However, voriconazole is often administered for longer durations where the accumulation can be significant. Will there be significant accumulation with a five day course? Should we be worried about potential accumulation and potential kidney injury, when facing a mortal illness (even if the medicine doesn’t seem to affect this mortality)?
Excluding patients with reduced kidney function as defined by the RCTs means that one would have to exclude patients with acute kidney injury, and those with CKD4 and 5, including patients on dialysis.
Acute kidney injury (AKI) is quite common, particularly in hospitalized patients. Among critically ill COVID patients, anywhere from 20 to 30% may develop AKI. Additionally, these patients do much worse than patients who do not have AKI. Similarly, patients with a GFR less than 30 have worse outcomes than those with preserved kidney function (see OpenSafely data, Williamson et al, Nature 2020).
Fig. 3 from Williamson et al : Estimated hazard ratios for each patient characteristic from a multivariable Cox model.
Among those who are on dialysis, the mortality is about 25%. A nice editorial summarizing recent data by Caroline Hsu and Dan Weiner is here. So why should we withhold a possibly effective drug in those who are at highest risk of dying? Why should we accept therapeutic nihilism for kidney patients?
In this study, the investigators wisely chose to ignore the prevailing wisdom, and decided to treat the patients based on their assessment of the evidence. Let’s see what happened.
The Study
This study is a single centre study encompassing patients with COVID-19 who had AKI or CKD; patients with all stages of AKI admitted to ICU and Nephrology between July (when Remdesivir became available in this centre) and September 2020. AKI was defined as per the 2012 KDIGO guidelines, ESRD was defined as irreversible loss of kidney function requiring dialysis for greater than 3 months
Primary outcome
Safety of remdisivir based on clinical and laboratory parameters
Clinical evaluation: heart rate, respiratory rate, blood pressure, orthostatics and focussed systematic examination
Laboratory evaluation: CBC, liver and renal profile, ABG, C reactive protein, LDH, IL-6, D dimer, ferritin
Chest X ray and high resolution CT scan of chest were performed for all patients.
Secondary outcomes
Duration of hospital stay
Mortality
Protocol
Patients were treated “per standard protocol” including respiratory support (depending on hypoxaemia), antibiotics, prophylactic anticoagulation and steroids
Severe COVID-19 was defined as O2 saturation <94% or those requiring oxygen. These patients were treated with IV remdesivir 200mg on day 1, followed by 100 mg daily for four consecutive days with therapy extended up to 10 days (per physician decision if indicated)
Patients were monitored clinically with vital monitoring including pulse oximetry, fluid balance assessment and cardiac monitoring. Renal and liver profiles were taken on days 0, 3, 5 and 7 of remdesivir therapy in all or daily if baseline AST/ALT abnormality.
Patients were evaluated twice daily by Nephrologists (three of the authors) examining the relevance of possible adverse events. This involved discussion of patient status and reporting according to the WHO-UMC scale
Criteria for dialysis initiation were refractory fluid overload, metabolic acidosis, hyperkalaemia, altered mental status (attributed to uraemia) or need for blood/blood product transfusions in the presence of oliguria. Dialysis modalities were either IHD or SLED dependent on patient status.
Results
157 patients with covid were admitted to the ICU in the authors’ nephrology high dependency unit.
46 were treated with remdesivir.
8 with kidney transplants
30 with AKI
3 with KDIGO stage 1
2 with KDIGO stage 2
25 with KDIGO stage 3
36 were on dialysis
16 ESKD
20 AKI
12 were in the ICU
Median age 53
Male:Female 65%:35%
Hypertension (76%) and diabetes (57%) were common in the remdesivir group.
Oxygen requirements
Remdesivir was given as 200 mg on day 1 and then 100 mg on days 2-5 for a total course of 600 mg. Two patients got a total of 1200 mg due to insufficient clinical response.
One patient had an infusion reaction that responded to steroids and antihistamines.
With respect to kidney function, among the patients with AKI, those who were dialysis remained dialysis dependent (except 2 who died). Among those who were not dialysis dependent, the kidney function either remained stable, or improved. See table below for details:
Table 2 from Thakare et al, KI Reports 2020
Discussion
The bottom line:
No significant abnormalities in renal function attributable to the drug were noted
No clinically significant ALT elevations
No early discontinuation of therapy due to adverse effects
Limitations:
Most of the patients were on HD therefore the authors cannot comment on safety in patients with CKD down to low GFR; This is not necessarily a limitation as the paper provides useful data on dialysis patients
Serum SBECD concentrations were not measured however SBECD accumulation did not correlate with a rise in creatinine
The aqueous form of remdesivir was used which has twice the concentration of SBECD than the powdered form of remdesevir
Lack of a control arm
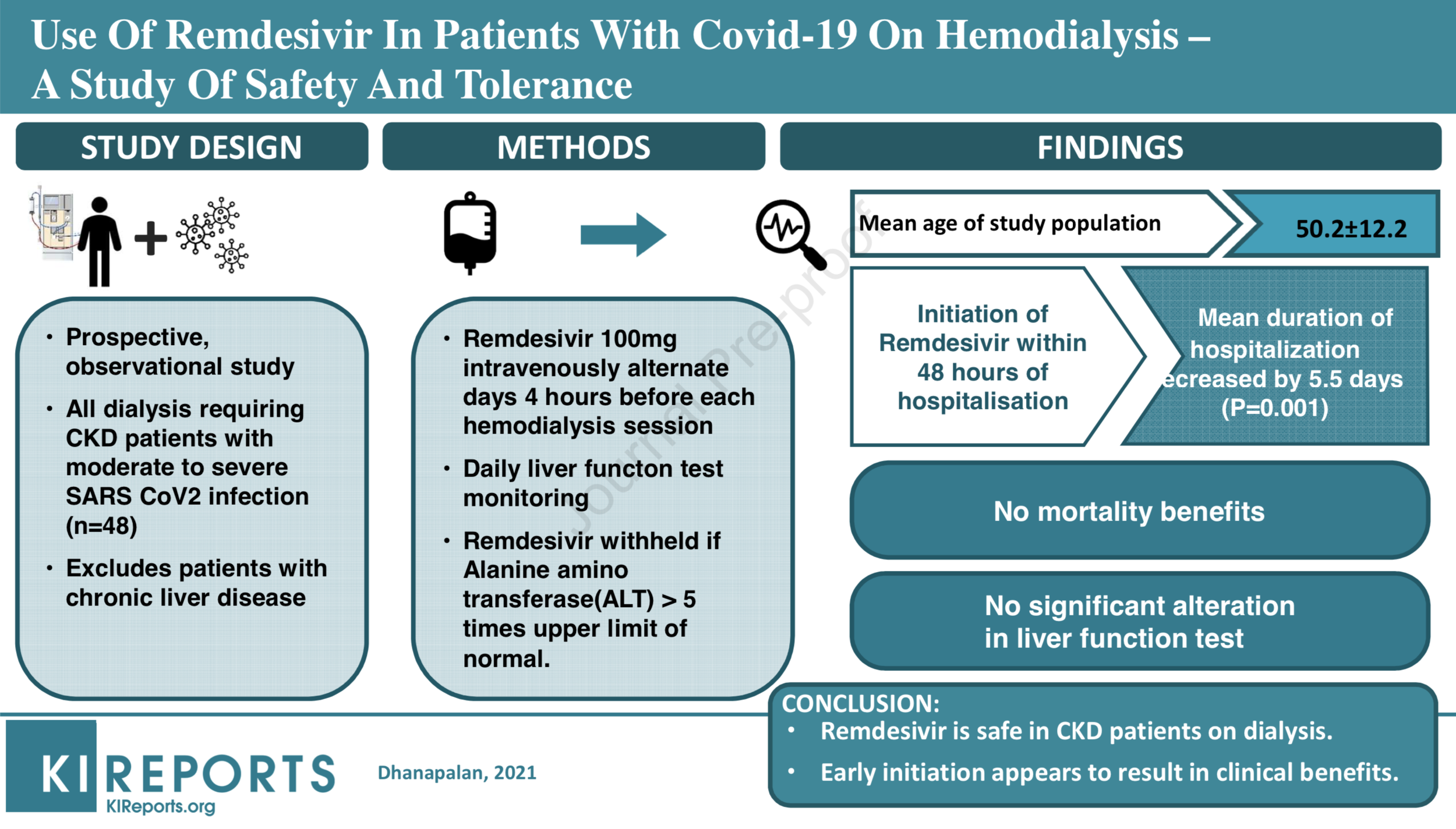
There have been a few other studies of Remdesivir since, see summary below:
Source: Thakare et al, KI Reports 2020; Estiverne et al, KI Reports 2020; Aiswarya et al, KI Reports 2020; Ackley et al, Antimicrobial Agents and Chemotherapy, 2020
Thus, overall:
there is no overt toxicity in patients already on dialysis (either AKI or ESKD)
there is no obvious nephrotoxicity in patients with GFR (either AKI or CKD) in the doses and duration used here
Evaluation of treatments for patients with AKI and CKD and COVID-19 remains an unmet clinical need and an urgency remains in further examining this issue due to the risk of morbidity and mortality in this group. This is the first report of remdesivir being used in patients with severely reduced kidney function and the data from this paper suggests it is tolerated well. The magnitude and unyielding pace of the COVID pandemic necessitates that we continue to recruit patients with AKI, CKD and ESKD to such trials to inform clinical decision making with a view to instituting potentially life-saving treatments in this patient group
Summary prepared by Swapnil Hiremath
with assistance from Joel Topf and Laura Slattery